
Our Intensive Care Unit (ICU) provides specialized, round-the-clock care for critical ailments. With state-of-the-art medical technology and a team of highly experienced Intensivists, Nurses and Specialists, we ensure the highest level of care and monitoring.
- Advanced Ventilator Support – For patients with Respiratory distress.
- Cardiac Monitoring – Continuous tracking of ECG, Blood Pressure and Oxygen Saturation for precise Heart health management.
- Specialized Intensive Care Team – Experienced Intensivists, Nurses and support staff.
- Infection Control Measures – Strict hygiene and sterilization protocols.
- Multi-Disciplinary Approach – Collaboration between specialists in pulmonology, neurology, cardiology, and more.
- 24/7 Emergency Response – Immediate medical attention for critical cases, ensuring life-saving interventions without delay.
Providing compassionate and expert care for critically ill patients—because every life matters.
Advanced Ventilator Support
For patients with Respiratory distress.
The Importance of Ventilator Support in Respiratory Distress
Respiratory distress is a critical condition in which the lungs cannot effectively perform gas exchange, leading to low oxygen levels (hypoxemia) and/or high carbon dioxide levels (hypercapnia) in the blood. It can result from conditions such as pneumonia, COVID-19, ARDS (acute respiratory distress syndrome), COPD exacerbations, or chest trauma. When conventional oxygen therapy is insufficient, advanced ventilator support becomes essential to stabilize the patient and support vital functions. This support helps relieve the workload on the respiratory muscles, maintain adequate oxygenation, and protect other organs from the effects of oxygen deprivation.
Types and Modes of Advanced Ventilator Support
Advanced ventilators offer a variety of settings and modes designed to match the needs of each patient. These include invasive ventilation via an endotracheal tube and non-invasive ventilation (NIV) using masks. Common modes include volume-controlled ventilation, pressure-controlled ventilation, and more sophisticated settings like SIMV (synchronized intermittent mandatory ventilation) or APRV (airway pressure release ventilation). These modes are adjusted to provide lung-protective ventilation, especially in patients with ARDS, to minimize lung injury while ensuring effective gas exchange. Proper mode selection and parameter settings are vital to avoid complications such as barotrauma and ventilator-induced lung injury.

Monitoring and Managing Complications
Effective ventilator support requires continuous monitoring and expert adjustment. Healthcare professionals track vital signs, blood gas levels, lung compliance, and airway pressures to ensure the patient is responding well to ventilation. Over time, complications such as ventilator-associated pneumonia (VAP), pressure injuries, and difficulty weaning from the ventilator can arise. Strategies such as regular oral care, early mobility, and spontaneous breathing trials help reduce these risks. It’s essential for a multidisciplinary team—including doctors, respiratory therapists, and nurses—to collaborate in managing the patient’s respiratory support and overall recovery.
Recovery and Advances in Ventilator Technology
As the patient’s condition improves, efforts shift toward weaning them from the ventilator and supporting full respiratory recovery. This process may involve gradually reducing ventilator support and transitioning to non-invasive options. In recent years, ventilator technology has advanced significantly, offering features like real-time monitoring, automated adjustments, and improved patient-ventilator synchrony. These innovations not only enhance patient safety but also improve comfort and outcomes. With ongoing development in respiratory care, advanced ventilator support continues to play a pivotal role in saving lives and facilitating recovery for patients with severe respiratory distress.

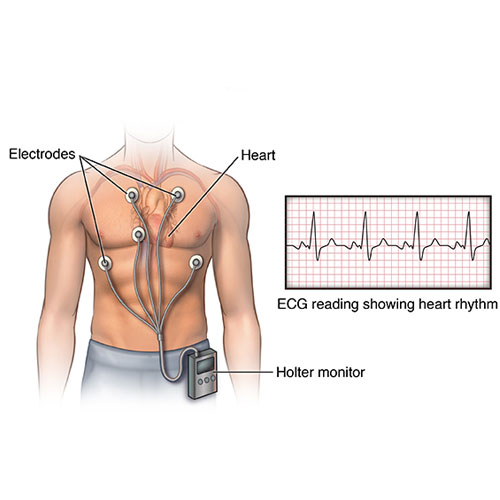
Cardiac Monitoring
Continuous tracking of ECG
Introduction to Cardiac Monitoring
Cardiac monitoring is a vital tool in modern healthcare, enabling the continuous observation of heart-related parameters such as electrocardiogram (ECG), blood pressure, and oxygen saturation. It plays a crucial role in both acute care settings, such as emergency rooms and intensive care units, and in long-term management of patients with chronic heart conditions. By closely tracking these indicators, healthcare professionals can detect abnormalities like arrhythmias, myocardial ischemia, or sudden drops in blood pressure early, allowing for prompt intervention and potentially life-saving treatment.
ECG Monitoring and Heart Rhythm Analysis
Electrocardiogram (ECG) monitoring is central to cardiac care, as it provides real-time data on the electrical activity of the heart. Continuous ECG monitoring can detect arrhythmias, myocardial infarctions, and conduction blocks that may otherwise go unnoticed. In critical care or post-operative settings, this data helps clinicians manage patients who are at risk of complications such as atrial fibrillation or ventricular tachycardia. Advanced systems also incorporate alarms and automated interpretation to alert caregivers immediately when abnormal rhythms are detected, enhancing patient safety.

Blood Pressure and Oxygen Saturation Monitoring
Blood pressure and oxygen saturation are equally essential components of cardiac monitoring. Continuous blood pressure monitoring helps assess cardiac output and vascular resistance, providing insights into the patient’s hemodynamic stability. Meanwhile, pulse oximetry continuously tracks oxygen saturation (SpO₂), ensuring that the heart and other vital organs are receiving adequate oxygen. These parameters are especially important in patients with heart failure, shock, or undergoing surgery. When monitored together with ECG, they offer a comprehensive picture of cardiovascular function.
Benefits of Continuous Cardiac Monitoring
Continuous cardiac monitoring allows for more precise and proactive heart health management. It enables healthcare providers to respond to changes before they become critical, improving outcomes and reducing hospital stays. For patients with chronic heart disease, wearable monitoring devices now make it possible to track heart health remotely, improving quality of life and reducing emergency visits. Overall, continuous cardiac monitoring is not just a diagnostic tool—it’s a cornerstone of preventive care, early intervention, and personalized heart health management.
Specialized Intensive Care Team
Experienced Intensivists, Nurses and support staff.
The Backbone of Critical Care
A Specialized Intensive Care Team is the cornerstone of effective treatment in the Intensive Care Unit (ICU). This highly trained group of professionals works around the clock to manage life-threatening conditions and ensure optimal outcomes for critically ill patients. Their combined expertise allows for quick, precise decision-making in high-pressure situations. These teams are equipped to handle a wide range of emergencies, from respiratory failure and sepsis to complex post-operative care, making their presence essential for patient survival and recovery.
Role of Intensivists in the ICU
Intensivists are physicians with specialized training in critical care medicine. They lead the ICU team and are responsible for developing and managing individualized treatment plans. Their expertise lies in understanding complex organ systems, advanced life-support technologies, and interpreting diagnostic tests to make rapid, evidence-based decisions. Intensivists play a pivotal role in coordinating care, communicating with families, and guiding patients through the most vulnerable phases of their medical journey.

Critical Care Nurses: Skilled and Vigilant
Critical care nurses are the front line of patient monitoring and hands-on care in the ICU. They are trained to detect even the slightest changes in a patient's condition and respond immediately. These nurses manage ventilators, administer intravenous medications, monitor vital signs, and provide emotional support to patients and families. Their role requires not only technical expertise but also compassion and resilience, as they often deal with high-stress, emotionally charged situations.
Multidisciplinary Support for Holistic Care
Beyond doctors and nurses, the ICU team includes a range of support staff such as respiratory therapists, physiotherapists, pharmacists, nutritionists, and social workers. Each plays a vital role in the patient’s recovery. Respiratory therapists manage ventilator settings and ensure proper airway support, while pharmacists fine-tune medication regimens. Physical therapists help prevent muscle atrophy and support mobility, and social workers assist families with emotional and logistical challenges. This collaborative approach ensures that patients receive comprehensive, high-quality care tailored to their unique needs.

Infection Control Measures
Strict hygiene and sterilization protocols.
Importance of Infection Control in Healthcare Settings
Infection control measures are a critical part of patient safety and hospital operations, especially in high-risk environments like intensive care units, operating rooms, and emergency departments. These measures are designed to prevent the spread of infections caused by bacteria, viruses, and other harmful microorganisms. Without strict protocols, healthcare-associated infections (HAIs) can quickly spread, putting patients, staff, and visitors at risk. Effective infection control not only protects vulnerable individuals but also reduces hospital stays, treatment costs, and the overall burden on the healthcare system.
Hygiene Practices and Handwashing Protocols
One of the most fundamental aspects of infection prevention is strict hand hygiene. Medical staff are required to wash or sanitize their hands before and after every patient interaction using approved handwashing techniques. Alcohol-based hand rubs are commonly used because they are quick and effective at killing most pathogens. Facilities also enforce the use of gloves, gowns, and masks when necessary, especially during procedures or while caring for patients with known infections. These practices drastically reduce the risk of cross-contamination between patients and staff.

Sterilization and Disinfection Procedures
Sterilization and disinfection of medical instruments, surfaces, and equipment are essential to infection control. All reusable tools undergo thorough cleaning, followed by sterilization using autoclaves or chemical disinfectants to eliminate any trace of infectious agents. High-touch surfaces, such as bed rails, monitors, and doorknobs, are cleaned frequently using hospital-grade disinfectants. Operating rooms, procedure areas, and ICUs follow rigid cleaning protocols between every patient, ensuring a sterile environment that meets health and safety standards.
Staff Training and Ongoing Compliance Monitoring
Maintaining strict infection control requires continuous education and monitoring. All healthcare workers undergo regular training on updated guidelines, outbreak management, and the correct use of personal protective equipment (PPE). Hospitals also employ infection control specialists who audit compliance, investigate outbreaks, and ensure that safety procedures are being followed consistently. With constant vigilance and commitment from all staff, infection control becomes a proactive defense that safeguards patient health and preserves the integrity of the healthcare environment.

Multi-Disciplinary Approach
Collaboration between specialists in pulmonology, neurology, cardiology, and more.
The Value of a Multi-Disciplinary Care Model
A multi-disciplinary approach in healthcare brings together experts from various specialties to deliver holistic and highly coordinated patient care. In complex or critical cases—such as those involving multiple organ systems or chronic conditions—this collaborative model ensures that all aspects of a patient's health are addressed. By integrating the expertise of pulmonologists, neurologists, cardiologists, intensivists, and other specialists, healthcare providers can form comprehensive treatment plans that are more effective and personalized. This approach is particularly essential in intensive care units (ICUs), where patients often face interconnected medical challenges.
Enhanced Decision-Making Through Collaborative Expertise
In a multi-disciplinary team, each specialist contributes their unique knowledge to the diagnostic and treatment process. For instance, a cardiologist may manage heart function while a pulmonologist oversees ventilator support, and a neurologist monitors cognitive or neurological changes. These specialists meet regularly to review the patient’s condition, interpret test results collectively, and adjust the care plan accordingly. This synergy improves diagnostic accuracy, prevents treatment delays, and minimizes the risk of oversight, especially in rapidly changing clinical situations.

Improved Patient Outcomes and Quality of Care
Studies consistently show that multi-disciplinary care leads to better patient outcomes, including shorter hospital stays, reduced readmission rates, and lower mortality in critical care settings. Patients benefit not only from medical expertise but also from the coordination between clinical care, rehabilitation, and psychosocial support. The presence of pharmacists, dietitians, physiotherapists, and mental health professionals further enhances recovery by addressing the full spectrum of patient needs—from nutrition and mobility to emotional well-being.
Communication and Coordination as Core Pillars
Effective communication is the backbone of any successful multi-disciplinary team. Structured team meetings, shared electronic health records, and standardized communication protocols ensure that every team member is informed and aligned with the treatment goals. Patients and their families are also considered part of the care team, as their input and understanding are crucial for informed decision-making and adherence to treatment plans. This collaborative environment fosters trust, transparency, and ultimately, a higher standard of care that treats the patient as a whole, not just a set of symptoms.

24/7 Emergency Response
Immediate medical attention for critical cases, ensuring life-saving interventions without delay.
The Critical Need for Around-the-Clock Emergency Response
Medical emergencies can strike at any time, and the availability of 24/7 emergency response services ensures that patients receive immediate care when it matters most. Whether it’s a heart attack, stroke, trauma, or respiratory failure, delays in treatment can result in irreversible damage or even death. A fully operational emergency response system guarantees that trained personnel, diagnostic tools, and life-saving interventions are always ready, regardless of the hour. This constant preparedness is a cornerstone of effective healthcare delivery in both urban hospitals and rural medical centers.
Rapid Triage and Early Intervention
When a patient arrives in the emergency department or is transported via ambulance, the first step is rapid triage—prioritizing treatment based on the severity of their condition. Emergency teams, including doctors, nurses, and paramedics, are trained to assess and stabilize critical cases within minutes. Early interventions, such as airway management, defibrillation, or administration of clot-busting drugs, can significantly improve survival rates. Time-sensitive protocols are in place to handle conditions like myocardial infarction (heart attack) and stroke, where every minute counts in preserving life and function.

Integration with Critical Care and Specialist Teams
24/7 emergency response systems are tightly integrated with intensive care units, surgical teams, and specialist departments such as cardiology, neurology, and trauma. Once a patient is stabilized, they are seamlessly transitioned to the appropriate care unit for continued treatment. This continuity ensures that patients benefit from both immediate intervention and long-term management, minimizing complications. Real-time communication between emergency teams and specialty units also enables the pre-activation of operating rooms or ICU beds, reducing delays in care.
Enhancing Community Trust and Outcomes
The availability of round-the-clock emergency care enhances public trust and encourages people to seek help without hesitation. Knowing that expert medical attention is just a call or short drive away reduces anxiety and improves response times in critical situations. Additionally, ongoing investment in emergency training, technology, and infrastructure further strengthens the healthcare system’s ability to respond to disasters, mass casualty events, and everyday emergencies. In the broader picture, 24/7 emergency response is not just a service—it’s a lifeline that saves countless lives every day.




